Abstract:
Researchers from Kanazawa University have used machine learning to predict which classes of chronic heart failure patients are most likely to experience heart failure death, and which are most likely to develop an arrhythmic death or sudden cardiac death. If confirmed in a larger study, these results will help doctors extend the life of patients worldwide.
Kanazawa, Japan – Tens of millions of people worldwide have chronic heart failure, and only a little over half of them survive 5 years beyond their diagnosis. Now, researchers from Japan are helping doctors to assign patients into groups based on their specific needs, to improve medical outcomes.
In a study recently published in the Journal of Nuclear Cardiology, researchers from Kanazawa University have used computer science to disentangle patients most at risk of sudden arrhythmic cardiac death from patients most at risk of heart failure death.
Doctors have many methods at their disposal for diagnosing chronic heart failure. However, there's a need to better identify what treatment to pursue, in accordance with the risks of each approach. When combined with conventional clinical tests, a molecule known as iodine-123 labelled MIBG can help discriminate between high-risk and low-risk patients. However, there is no way to assess the risk of arrhythmic death separately from the risk of heart failure death, something the researchers at Kanazawa University aimed to address.
"We used artificial intelligence to show that numerous variables work in synergy to better predict chronic heart failure outcomes," explains lead author of the study Kenichi Nakajima. "Neither variable, in and of itself, is quite up to the task."
To do this, the researchers examined the medical records of 526 patients with chronic heart failure and who underwent consecutive iodine-123-MIBG imaging and standard clinical testing. Conventional medical care proceeded as normal after imaging.
"The results were clear," says Nakajima. "Heart failure death was most common in older adult patients with very low MIBG activity, worse New York Heart Association class, and comorbidities."
Furthermore, arrhythmia was most common in younger patients with moderately low iodine-123-MIBG activity and less serious heart failure. Doctors can use the Kanazawa University researchers' results to tailor medical care; for example, the type of implantable defibrillator most likely to meet the needs of the patient.
"It's important to note that our results need to be confirmed in a larger study," explains Nakajima. "In particular, the arrhythmia outcomes were perhaps too infrequent to be clinically reliable."
Given that chronic heart failure is a global problem that frequently kills within a few years after diagnosis, if not treated appropriately, it's essential to start the most appropriate medical care as soon as possible. With a reliable test that predicts which patients most likely need which treatments, a greater number of patients are likely to live longer.
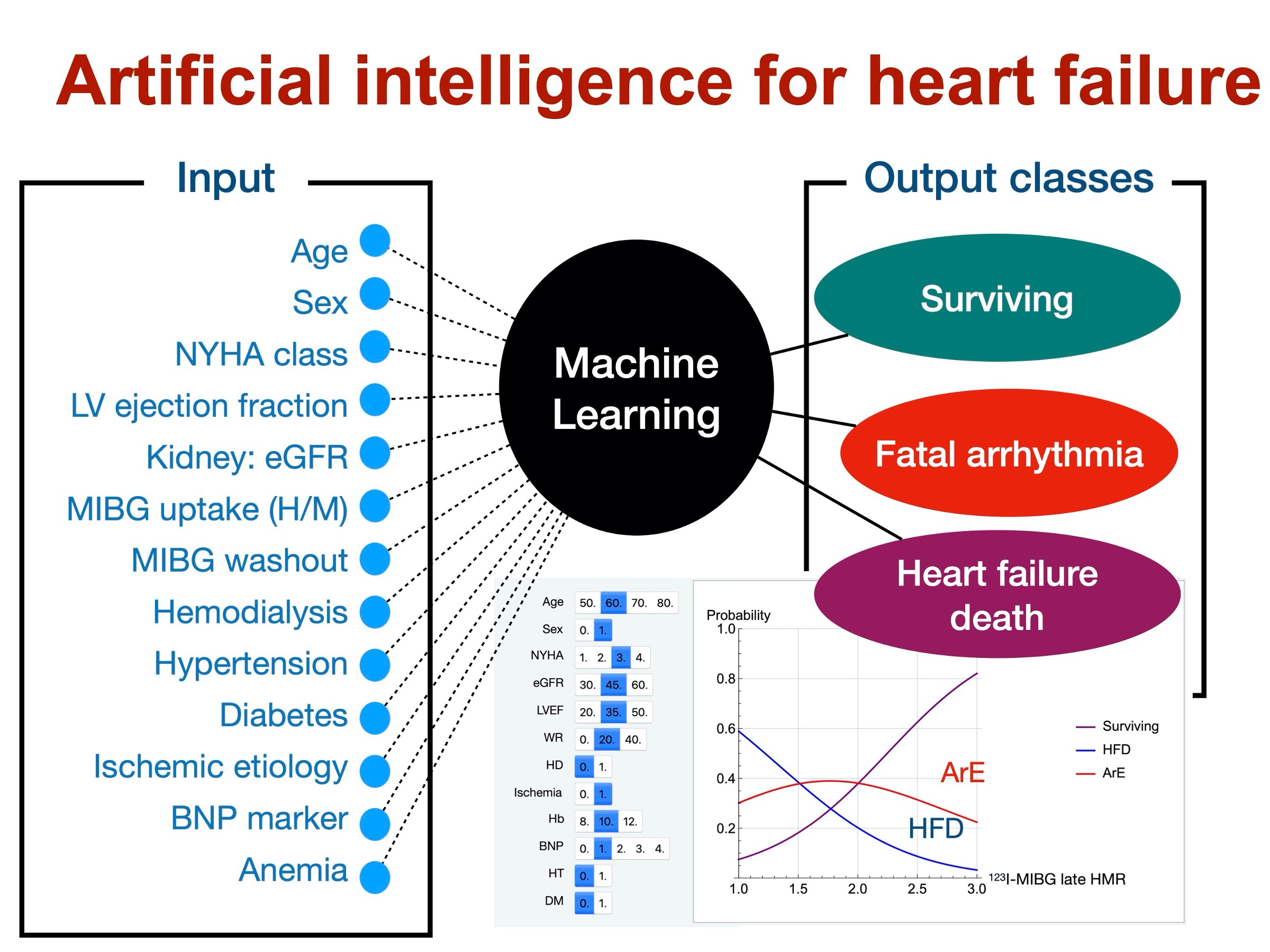
Figure1
Machine learning uses 13 input data to predict fatal arrhythmia (sudden cardiac death), heart failure death and survival.
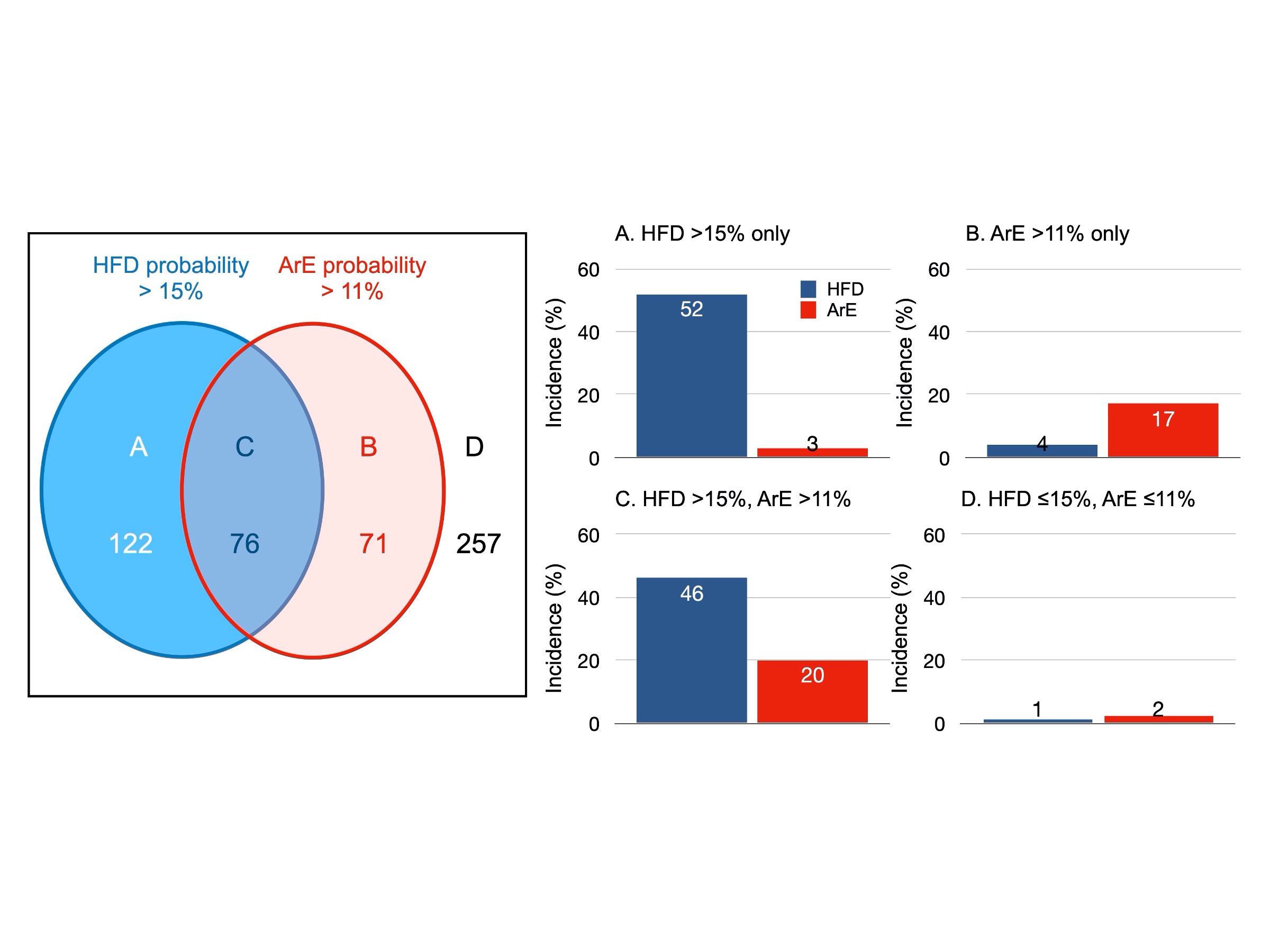
Figure2
Patients with high and low probabilities of heart failure death (HFD) and fatal arrhythmic events (ArE). High-risk patients for HFD and ArE actually showed high incidence of each outcome, while low-risk patients did survive without any events.
Article
Machine learning-based risk model using 123I-metaiodobenzylguanidine to differentially predict modes of cardiac death in heart failure
Journal:Journal of Nuclear Cardiology
Authors:Kenichi Nakajima, Tomoaki Nakata, Takahiro Doi, Hayato Tada, Koji Maruyama



 PAGE TOP
PAGE TOP