Abstract:
We revealed that ALK-positive lung cancer cells, treated with crizonitib, a molecular target drug, acquired resistance to the drug not only by genetic mutation but also by concomitant epithelial-to-mesenchymal transition (EMT). Further, in animal experiments, mesenchymal cancer cells due to EMT were shown to revert to epithelial ones by quisinostat, a histone deacetylase (HDAC) inhibitor; they regained sensitivity to the molecular-targeted drug. These results indicate a significant potential of overcoming resistance to molecular-targeted drugs in ALK-positive lung cancer.
[Background]
Although molecular-targeted drugs*1) have been known to show high efficacy to lung cancer patients, they also have limitations due to acquiring resistance to the drug used. Recurrence of target tumors may therefore take place, which is a serious problem (Figure 1). It has been well recognized that genetic mutation is somehow induced in the cancer cells on which the molecular-targeted drug is effective and that consequently, the structure of the target molecule of the cancer cell is changed; thus the cancer cell acquires resistance. In addition to genetic mutation, it has recently been suspected that epithelial-to-mesenchymal transition (EMT)*2) is another mechanism for cancer to acquire such resistance. However, the detailed relationship between EMT and drug resistance has not been elucidated, and medical treatments to overcome such problems have not been established.
[Outline of research results]
The present research team at Kanazawa University analyzed tumor tissues from patients with ALK-positive lung cancer*3) that acquired resistance to crizonitib, a molecular-targeted drug. As a result, it was revealed that a part of the tumor lesion developed a genetic mutation while another part underwent EMT. It was therefore thought that genetic mutation(s) and EMT should be individually responsible for the resistance against the molecular-targeted drug (Figure 2).
Next generation molecular-targeted drugs that should overcome genetic mutation problems have already been used clinically, whereas no therapeutic means have been developed for the resistance due to EMT. The team investigated the mechanism for inducing cancer cell EMT. As a result, it was found that cancer cells acquired resistance to the molecular-targeted drug by transforming epithelial characteristics into mesenchymal ones, caused by reduction in the cancer cells of the expression of miR-200c (one of the microRNAs that regulate gene expression). Reduction of miR-200c expression augments the level of ZEB1, a transcription factor that induces EMT, and reduces the level of E-cadherin, a protein involved in cell adhesion.
Next, the team searched for compounds that could augment the expression of miR-200c to normal levels, in the hope that the resistance could be overcome by possible reverse-transition of mesenchymal cancer cells into epithelial ones. As a result, treatment with an HDAC (histone deacetylase) inhibitor*4), quisinostat, reversed the transformation of mesenchymal cancer cells into epithelial cells, which led to successful sensitization of the resultant cells to molecular-targeted drugs (Figure 3).
In addition, it was revealed in animal experiments that acquisition of cancer cell resistance to the molecular-targeted drug was evidently prevented by quisinostat treatment prior to the drug treatment.
From these results, sequential treatment with quisinostat, an HDAC inhibitor, followed by a next generation molecular-targeted drug may have a big potential for overcoming resistance to molecular-targeted drug by ALK-positive lung cancers due to genetic mutation and EMT (Figure 4).
[Future prospects]
Due to these results, it is now expected that patients with a cancer demonstrated to have EMT and resistance against targeted drugs may be, by overcoming such resistance, completely cured or may have a significant delay of cancer recurrence by sequential treatment with an HDAC inhibitor and a next generation molecular-targeted drug.
The team will now investigate the selection of the best HDAC inhibitor in terms of efficacy and adverse effects as well as the clinical examination of therapy in combination with next generation molecular-targeted drugs.
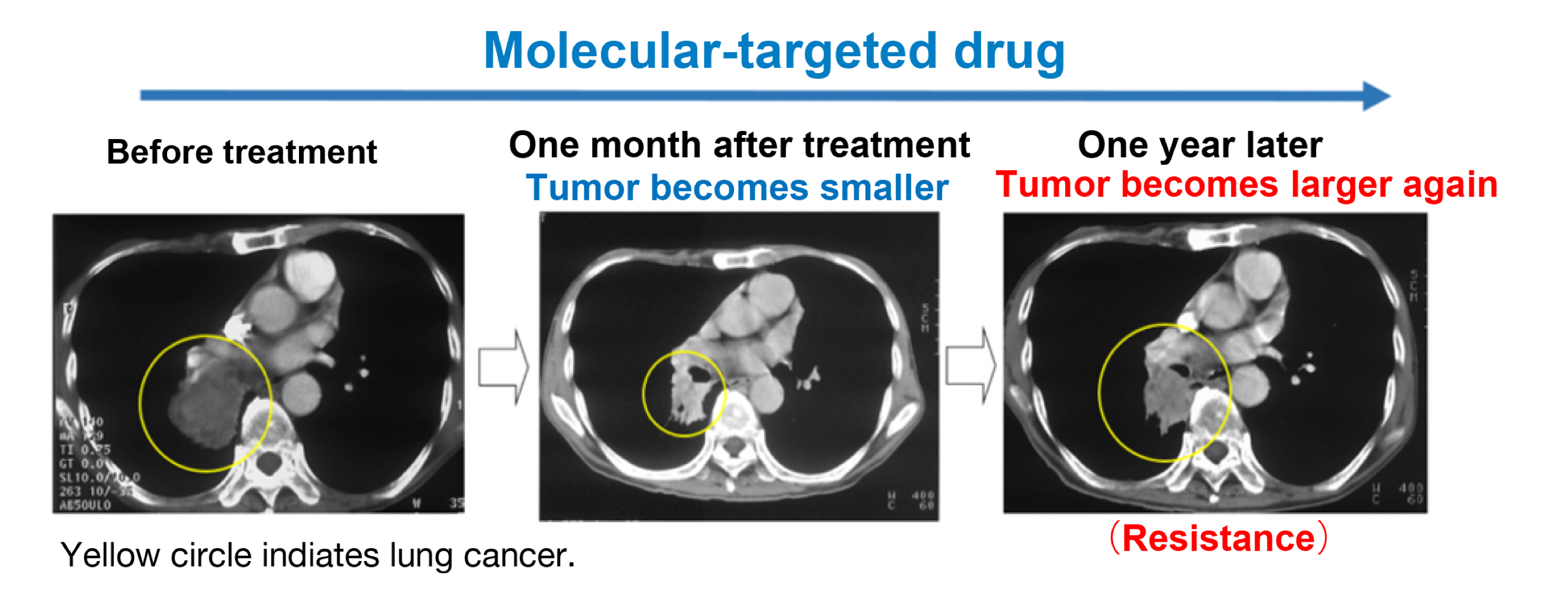
Figure 1.
Molecular-targeted drugs are effective for a while, but a part of the tumor lesion survives to recur.
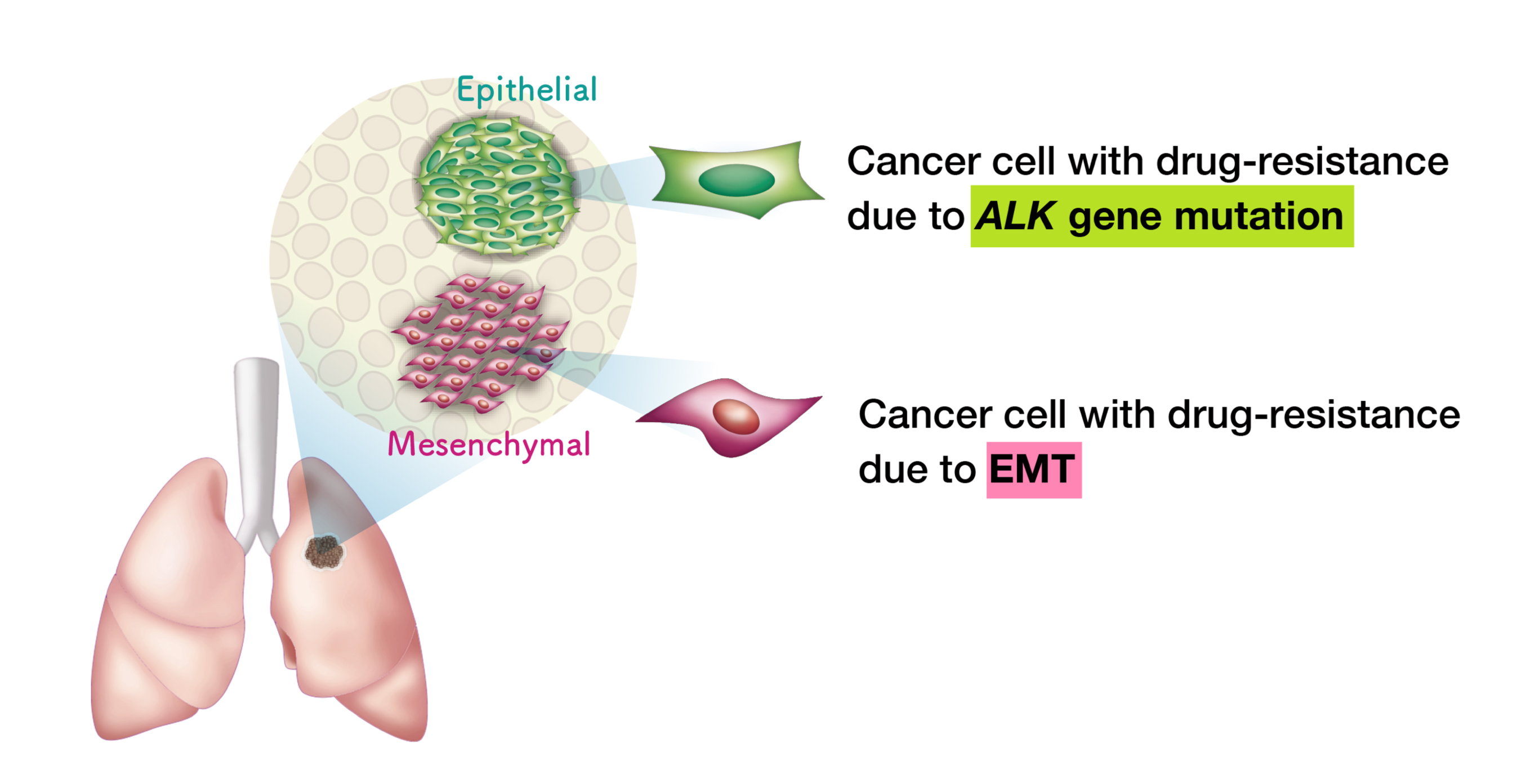
Figure 2.
In tumor tissue of an ALK-positive lung cancer patient who has acquired resistance to molecular-targeted drug, a part with ALK-positive genetic mutation and a part with EMT resistance coexist.
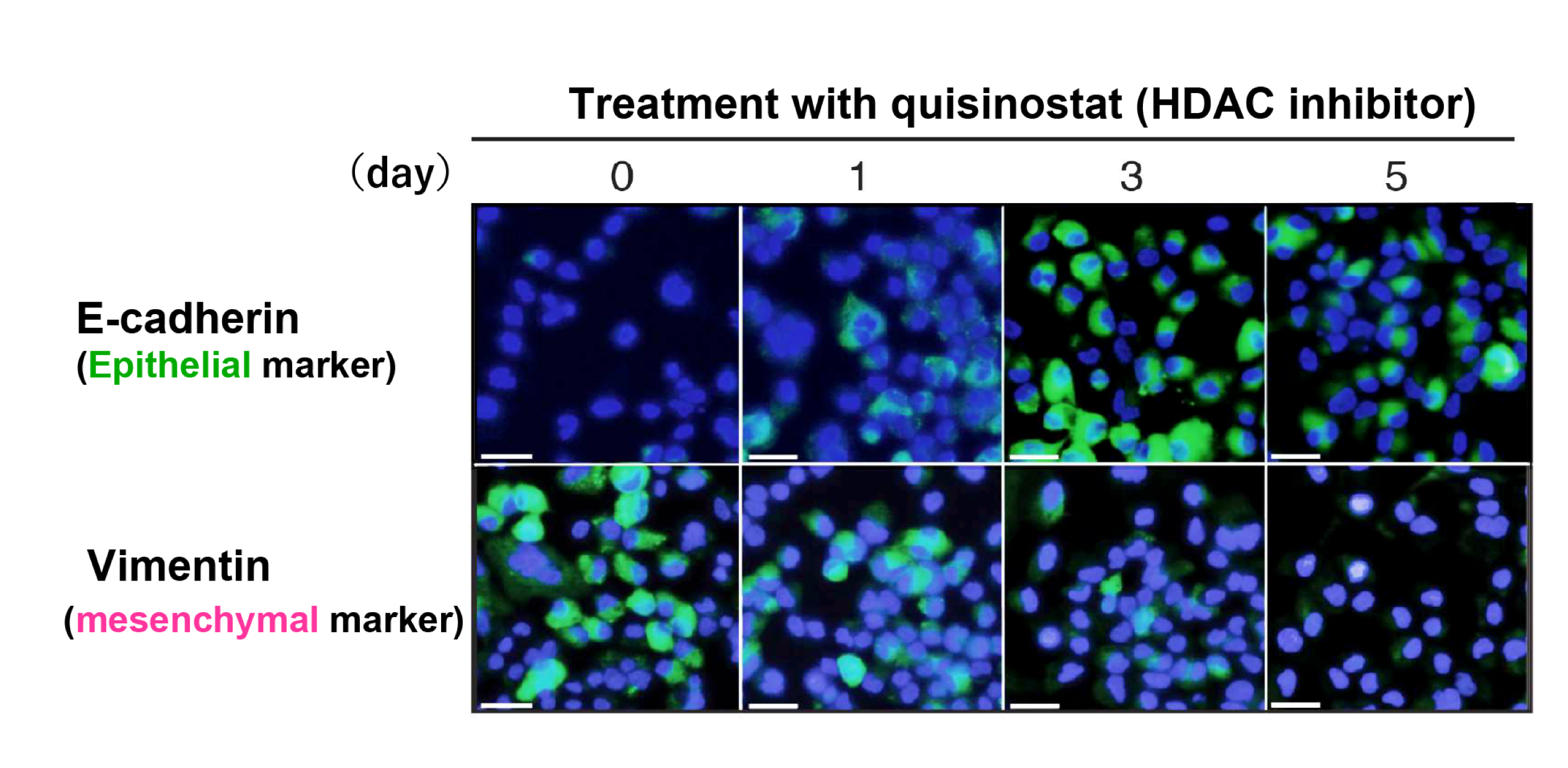
Figure 3.
Reverse-transition to epithelial characteristics by quisinostat treatment of ALK-positive lung cancer cells that had acquired resistance to crizonitib, a molecular-targeted drug (the epithelial marker was augmented while the mesenchymal marker decreased).
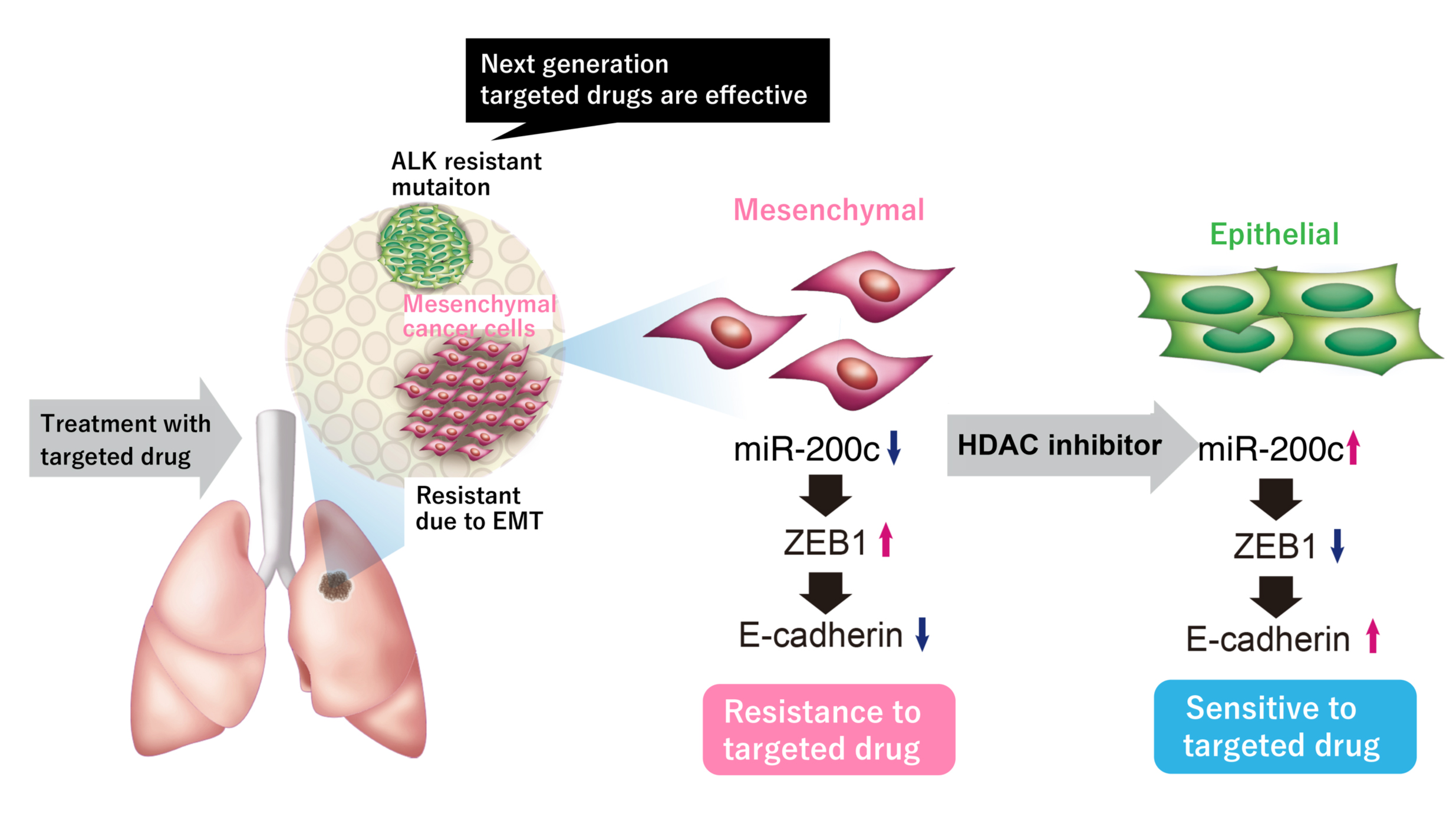
Figure 4.
Treatment of mesenchymal cancer cells with an HDAC inhibitor induces augmentation of the expression level of miR-200c, which then induces reverse-transition of the cancer cells to restore epithelial characteristics; such cancer cells with reverse-transition are now sensitive to molecular-targeted drugs.
[Glossary]
*1) Molecular-targeted drug
A molecular-targeted drug acts on a specific molecule that plays an important role in cancer proliferation and survival. In 2001, imanitib (brand name, Gleevec) against leukemia and trastudumab (brand name, Herceptin) against breast cancer were approved for clinical usage for the first time as molecular target drugs. Nowadays, more than 40 such molecular-targeted drugs are approved for cancer treatment in Japan.
*2) Epithelial-to-mesenchymal transition (EMT)
Epithelial-to-mesenchymal transition (EMT) is a process by which epithelial cells lose their cell polarity and cell-cell adhesion ability, and gain invasive properties to become mesenchymal cells. EMT is reported to be involved in cancer metastasis and the acquisition of drug resistance.
*3) ALK-positive lung cancer (ALK fusion gene positive lung cancer)
ALK-positive lung cancer is induced by fusion of the ALK (anaplastic lymphoma kinase) gene with another gene such as EML4, and accounts for about 5% of the Japanese non-small cell lung cancer patients. The ALK-positive lung cancer cells survive and proliferate due to signaling from the ALK-fusion protein. ALK tyrosine kinase inhibitor, a molecular target drug, is quite effective against this type of cancer.
*4) HDAC (histone deacetylase) inhibitor
Histone is a basic protein that plays important roles in condensing DNA. Functions of HDAC include prevention of the expression of genes that control cancer cell mitosis and cell morphology. In multiple myeloma, the level of HDAC activity is observed to be abnormally high, and therefore HDAC inhibitors are expected to exert anti-tumor effects.
Article
Epithelial-to-mesenchymal transition is a mechanism of ALK inhibitor resistance in lung cancer independent of ALK mutation status
Journal: Cancer Research
Authors: Koji FUKUDA, Shinji TAKEUCHI, Sachiko ARAI, Ryohei KATAYAMA, Shigeki NANJO, Azusa TANIMOTO, Akihiro NIDHIYAMA, Takayuki NAKAGAWA, Hirokazu TANIGUCHI, Takeshi SUZUKI, Tadaaki YAMADA, Hiroshi NISHIHARA, Hironori NINOMIYA, Yuichi ISHIKIWA, Satoko BABA, Kengo TAKEUCHI, Atsushi HORIIKE, Noriko YANAGITANI, Makoto NISHINO, and Seiji YANO
DOI: 10.1158/0008-5472.CAN-18-2052
Funder
JSPS KAKENHI 16K19447 and 18K07261.



 PAGE TOP
PAGE TOP